In 2026, healthcare providers offering medical billing services in USA are managing with a more complex system of claim denials than ever before. The rise in medical billing denial codes is not only an actual problem but also an economic and administrative one that can influence revenue and care for patients. Every denied claim may delay payments, increase paperwork, and create frustration for billing professionals. Stricter payer policies, better auditing systems, and new documentation and coding standards are all represented in the increasing amount of denial codes.
As reported by the American Hospital Association (AHA), U.S. hospitals and health systems have reportedly collectively spent an estimated $19.7 billion in appeals of denied billing in 2022 alone, with rejected claims involving costly services with an average claim payment exceeding $14,000. The AHA further states that “about 14.8% of all claims for private payers” and “15.7% for Medicare Advantage” and “13.9% for commercial” claims are denied in advance in order to cover certain services. This blog will explore common denial codes in 2026.
Evolving Trends in Denial Codes
Data that has been recently collected display that claims denials have increased significantly due to stricter payer compliance rules, electronic claim processing, and shifting reimbursement models. These trends have led to the introduction of updated denial codes that healthcare professionals must be aware of. In actuality, the list of denial codes in medical billing has extended to include more specific reasons related to documentation accuracy, pre-authorization issues, and coding precision. Healthcare providers who fail to track these changes:
- Risk higher denial rates
- Delayed reimbursement
- Interrupted cash flow especially as payers increasingly upgrade their claim review systems.
Why Understanding Denial Codes Matters
Learning the usual denial codes in medical billing is more about prevention not just correcting the errors. When medical billers comprehend what causes a denial, they can plan better workflows and educate medical staff to avoid repeated mistakes.
For example:
- The CO denial codes like CO-16 or CO 222 denial code (are common culprits in 2026.
- Identifying these patterns helps healthcare practices fix issues before claims reach payers, guaranteeing quicker reimbursements and less administrative burden.
Healthcare organizations can increase efficiency, minimize revenue losses, and create stronger payer relationships by staying ahead of medical denial codes.
The Influence of Policy and Compliance Changes
Both regulatory updates and payer policies play a major role in the increasing volume of denial codes for medical billing. Each year, insurers improve their standards for medical necessity, documentation standards, and prior authorization requirements. These modifications have led to new forms of common denial codes in 2026, mostly for telehealth, bundled services, and specialized procedures.
A highly proficient team of medical billing and revenue cycle experts especially within a Medical coding company in USA must remain active, continuously updating their systems and training to reflect the newest medical billing denial codes. This not only protects revenue but also ensures that patients experience fewer billing-related issues.
What Are Denial Codes?
In simple terms, denial codes in medical billing are standardized codes utilized by health insurance companies that describe why a medical claim was not paid in full or denied completely. Every denial code expresses a story. It helps healthcare providers to identify the root cause of the problem.
These medical denial codes are used as an important method of communication between payers and healthcare providers. It would be nearly impossible to locate where a claim failed, delaying payments and producing confusion for both billing teams and patients without medical denial codes.
Purpose of Denial Codes in Medical Billing
The purpose of denial codes for medical billing are to bring clarity and dependability to claim adjudication. Insurance companies can swiftly categorize the reason behind every rejection by assigning specific numeric or alphanumeric codes. This helps medical billers and RCM professionals take corrective actions with precision. According to the Centers for Medicare and Medicaid Services if you would not pay a claim for medical services, you have rights to appeal through outsourcing or directly connecting.
For example:
- CO-16: Incomplete or missing information.
- CO-97: Service included in another payment or bundled claim.
- CO 222 denial code: Exceeds the maximum number of allowed occurrences.
These standardized codes permit billing teams to address errors professionally, ensuring that claims are corrected, resubmitted, and paid without pointless delay.
Understand the Difference Between CARC and RARC
When discussing the list of denial codes in medical billing, two main groups appear. CARC and RARC.
- CARC: Stands for Claim Adjustment Reason Codes. These codes specify why the payment was adjusted or denied.
For example: CO-50 shows that the service is not covered by the policy of payer.
- RARC: Stands for Remittance Advice Remark Codes. These codes offer reasons for the denial or more background knowledge.
For example: an RARC might describe that more documentation is required to process the claim.
CARC and RARC codes form a complete explanation together that helps healthcare providers fully comprehend and resolve claim issues.
Pro Tip: Always carefully analyze both CARC and RARC codes together when a claim is denied. CARC codes identify the exact reason for denial, while RARC codes provide additional context or instructions. Understanding both confirms faster claim corrections, reduces resubmission errors, and helps maintain steady cash flow for your healthcare practice.
How Denial Codes Help Identify Billing and Documentation Issues
Denial codes do more than reject claims, they educate billing. Healthcare practices can uncover recurring documentation or coding errors that lead to lost revenue teams by analyzing patterns in medical billing denial codes.
For example:
- Frequent CO denial codes related to missing documentation might highlight a gap in clinical charting.
- Multiple CO 222 denial codes could indicate errors in claim entry or batching.
Healthcare providers increase the accuracy of their documentation and prevent future denials by analyzing these patterns.
Top 10 Most Common Denial Codes in 2026
In 2026, the complex system of denial codes in medical billing services in USA will keep continuing changing as insurance companies update their rules and regulations, digital audits, and policies for medical necessity. Understanding the most common denial codes in medical billing really helps to avoid claim rejections and protect revenue for healthcare providers.Repeated denials can be prevented by being mindful of particular issues with the billing or documentation process that are identified in each of these medical denial codes.
| Denial Code | Description |
| CO-16 | Claim is missing required details such as patient info, NPI, or supporting records. |
| CO-50 | Service is not covered under the patient’s insurance benefits. |
| CO-97 | Procedure is considered part of another already-paid service. |
| CO-109 | Claims were sent to the wrong insurance payer or billed out of order. |
| CO-18 | Same service for the same date and provider was already processed. |
| CO-29 | Claim was submitted after the payer’s allowed filing timeframe. |
| CO-151 | Documentation does not justify medical necessity for the billed service. |
| CO-197 | Required prior authorization was not obtained before service delivery. |
| CO-204 | Insurance plans exclude coverage for the billed service or item. |
| CO-252 | Provider NPI, taxonomy, or credentialing data is incomplete or incorrect. |
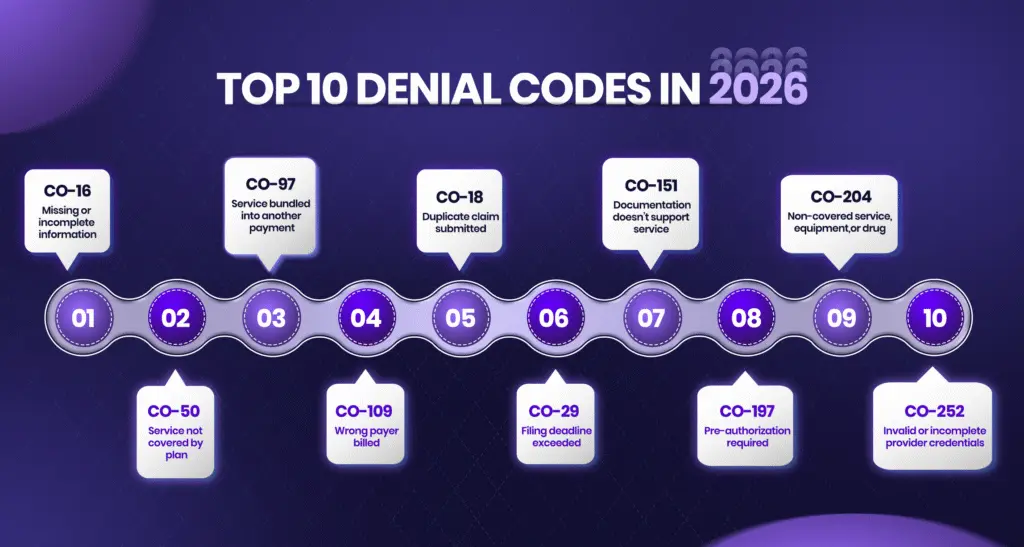
Below is the updated list of denial codes in medical billing that are most frequently observed in 2026.
1. CO-16 – Incomplete Information or Documentation
This is one of the most common CO denial codes. It occurs when a claim fails to include important data, such as a patient’s ID, the provider’s NPI, or any extra records, that include lab results or surgical notes. Making sure every field is complete before submission can considerably reduce this type of denial.
2. CO-50 – Non-Covered Services Under Payer Policy
This medical billing denial code shows that the submitted service is not covered by the insurance plan of a patient. Often related to benefit limitations or non-covered cosmetic or preventive procedures, these denials can be prevented through pre-verification of patient benefits and payer-specific policies.
3. CO-97 – Bundled or Included in Another Service
The CO-97 denial occurs when a billed procedure is considered part of another service that has already been paid. This denial mostly happens due to improper use of modifiers and entity codes in medical billing. Reviewing payer-specific bundling edits before billing is important to preventing these denials.
4. CO-109 – Claim Not Covered by This Payer or Contractor
This denial code comes when the claim is sent to the wrong payer or secondary insurance should have been billed instead. Avoid unnecessary claim denials by updating the latest insurance information and checking benefit coordination.
5. CO-18 – Duplicate Claim or Service
A CO-18 denial means that a similar claim for the same service, date, and healthcare provider has already been processed. Duplicates often result from system errors or accidental re-submissions. Implementing claim-tracking software helps detect duplicates before submission.
6. CO-29 – The Time Limit for Filing Has Expired
This denial code for medical billing is issued when a claim is submitted after the payer’s filing deadline. Payers have different timeframes for timely filing, which vary from 90 days to a year. Constant tracking of claim submission dates guarantees compliance and prevents revenue loss.
7. CO-151 – Information Does Not Support This Service
When the payer decides that the documents submitted do not support the billed service’s medical necessity, this code is generated. Proper clinical documentation and clear relationship between diagnostic and procedure codes are both essential to avoid this denial.
8. CO-197 – Precertification or Authorization Required
A CO-197 denial means that pre-authorization or pre-certification was not obtained before providing the service. These medical billing denial codes are common in radiology, surgeries, and high-cost treatments. These errors can be reduced by employing pre-authorization checklists prior to scheduling.
9. CO-204 – Service, Equipment, or Drug Not Covered
This denial indicates that the paid service, device, or prescription will not be covered by the insurance plan of a patient. Make sure you have insurance before initiating any procedures, particularly when you use pricey medical equipment or professional medications.
10. CO-252 – Incomplete or Invalid Credentialing/Provider Information
The CO 252 denial code occurs when the provider’s credentialing data such as NPI, taxonomy, or contract status is missing or incorrect. Keeping credentialing records updated with payers confirms smooth claim processing and reduces administrative denials.
Pro Tip: Constantly track the most frequent denial codes like CO-16, CO-50, and CO-97, and perform preventive checks prior to claim submission. Provide complete documentation, check patient coverage, check pre-authorizations, and keep updated provider credentials. Proactive attention to these problems may significantly decrease denials, accelerate up payments, while safeguarding the financial health of your practice.
Emerging Denial Patterns in 2026
Across the landscape of medical billing denial codes, 2026 ushers in a new era that includes automated processes, analytics, and evolving payer expectations. New categories of denials are developing for healthcare providers, often led on by artificial intelligence (AI) and analytical algorithms as technology alters the revenue cycle. Understanding these common denial codes in 2026 helps healthcare practices stay one step ahead, guaranteeing precision, compliance, and consistent cash flow. You can better understand denial codes by exploring outsource denial management services.
Telehealth Claims Face New Reimbursement Barriers
The continued growth of telehealth and performance driven reimbursement models has introduced new challenges in denial codes for medical billing. Many telehealth claims in 2026 are denied due to incorrect location coding, lack of documentation proving patient eligibility, or payer rules for telehealth services.
Similarly, results centered care models where reimbursement depends on outcomes rather than volume have given rise to medical billing denial codes related to incomplete quality metrics or missing performance data. Common examples include:
- Claims rejected for lack of quality measure submissions.
- Denials due to missing patient consent for telehealth visits.
- Errors in procedure codes for remote patient monitoring.
Staying updated with compliance requirements and payer telehealth policies can significantly reduce these denials.
Influence of CMS Updates and Payer Automation
Denial codes in medical billing are assigned according to updates from the CMS about documentation and billing processes. CMS updates have placed stronger emphasis on precise coding for preventive services, chronic care management, and remote monitoring.
Automation across payer systems also means that claims are now cross-verified against databases in real time leading to faster yet more frequent denials. Codes such as CO-16 and CO 222 denial code are being flagged more often due to systematic field verification.
Healthcare providers have to make sure their billing and EHR systems are up to date with most current CMS and payer regulations in order to cope. Rejections carried about by these new automated procedures can be minimized through the use of advanced claim-scrubbing tools, audits of compliance, and regular staff training.
Root Causes Behind Frequent Denials
In medical billing, each refusal code has a backstory. It may represent an insignificant error, an ignored detail, or a lately adopted rule that was not understood completely. Dealing with the root causes is the first step in reducing medical billing denial codes. The following are the root causes behind frequent denials.
1. Documentation and Coding Errors
Incomplete or inconsistent documentation remains one of the leading causes of common denial codes in medical billing. When a provider’s notes fail to support the billed service, claims are flagged for review or outright denial.
For example:
- CO-151 (information does not support this service) frequently results from vague or missing clinical notes.
- CO-16 (missing information) occurs when essential data—like diagnosis codes or service details is left incomplete.
Proper documentation not only supports coding accuracy but also aids justify the medical necessity of each service. Investing in coder training and electronic health record (EHR) audits can significantly reduce these denials.
2. Lack of Pre-Authorization or Eligibility Verification
In 2026, one of the primary causes of medical denial codes is missing pre-authorization. Payers increasingly demand prior authorization for specific medical products, tests, and medical procedures. Failing to obtain this approval leads to CO-197 denials. Similarly, missing or outdated insurance eligibility checks can lead to CO-109. These issues are entirely avoidable through instant coverage validation solutions that confirm eligibility immediately.
3. Incorrect Modifiers or Medical Necessity Issues
Another common culprit behind denial codes for medical billing is the misuse or omission of modifiers. Incorrect modifier combinations or failure to link them properly to procedure codes can lead to CO-97 or CO-50 denials. Consistent internal audits help ensure claims meet medical necessity standards and reduce these rejections.
4. Payer-Specific Rule Changes in 2026
Insurance carriers are gradually updating coverage guidelines, bundling rules, and Payer approval lists. These changes directly influence the list of denial codes in medical billing, introducing new or modified CO codes. For instance, CO 222 denial codes have risen as the result of modifications in chronic care management, durable medical equipment (DME) billing, and telemedicine coverage.
How to Interpret and Appeal Denial Codes
When a claim gets denied, it is not the end of reimbursement, it is the start of recovery. In 2026, healthcare providers must have the ability to read, understand, and strategically challenge denials due to the increasing complexity of denial codes in medical billing.
Pro Tip: Keep the billing system and EHR up to date and educate your staff on the most recent CMS rules, insurance policies, and telehealth requirements. Check patient eligibility and pre-approvals, examine documentation frequently and confirm modifiers are employed appropriately. Recognizing the reasons behind every denial code aids in preventing errors, simplifies appeals, and promises regular revenue in 2026.
Step-by-Step Process for Analyzing EOBs
Every denial initiated with an Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA) from the payer. These list the denial codes for medical billing, reasons, and payment breakdowns.
1. Identify the Denial Code
2. Read the Remark (RARC)
3. Verify Claim Info
4. Check Payer Policies
5. Document Findings
Inspecting EOBs helps teams identify recurring medical billing denial codes and decide which can be fixed quickly versus those needing full appeals.
How to Prepare Effective Denial Appeal Letters
Baseless denials can be reversed with an effective appeal.
- Be Specific: Describe why reconsideration is proper and provide the exact denial code observed in medical billing.
- Attach Documentation: Add clinical notes, operative reports, or pre-authorization proof.
- Stay Professional: Utilize short, factual language.
- Cite Guidelines: Reference CMS or payer policy sections.
- Meet Deadlines: Submit within 30–90 days.
Clear, well supported appeals increase reversal chances and show professionalism.
Best Practices for Tracking and Categorizing Recurring Denials
Efficient denial management reduces repeat issues.
- Maintain a Denial Log: Monitor each medical billing denial code, payer, and reason.
- Categorize by Type: Group by documentation, authorization, coding, or payer rules.
- Automate Reporting: Utilize RCM software to flag and report common denial codes in medical billing.
- Review Monthly: Discuss top denials, root causes, and prevention steps.
Constant tracking keeps denial patterns visible and manageable.
Tools and Strategies to Prevent Denials
Avoiding denial codes in medical billing before they occur is far more effective than appealing them later. In 2026, healthcare practices use intelligent automation, AI, and constant training to reduce errors and improve the accuracy of claims. The precise tools and proactive strategies help minimize the most common denial codes in medical billing, guarantee timely reimbursements, and strengthen revenue flow.
AI-Based Claim Scrubbing and RCM Automation
Artificial intelligence is altering medical billing denial code management. AI-based claim scrubbing tools thoroughly review claims before submission, checking for missing data, incorrect codes, and payer mismatches. These tools catch issues that cause common denial codes in medical billing like CO-16 or CO-15. In order to find high-risk claims and recommend solutions, Revenue Cycle Management (RCM) automation assesses historical medical billing denial codes via predictive analytics. This minimizes rejections, accelerates payments, and reduces medical billing denial codes.
Denial Management Dashboards in Billing Software
Real-time visibility is key to controlling denial codes in medical billing. Innovative billing software now includes dashboards that monitor live claim status, payer trends, and reasons of denial.
Key benefits:
- Categorize which CO denial codes occur most often and why.
- Picture data by payer, provider, or service.
- Assign follow-ups directly through the dashboard for quicker resolution.
These dashboards make denial management clearer and more effective.
Coder Training, Compliance Audits, and Payer Communication
Highly skilled staff are key to avoiding medical billing denial codes. Consistent coder training makes sure accuracy with payer rules and CMS updates. Compliance audits catch errors leading to medical billing denial codes like CO-50 or CO 222 denial code. Strong payer communication decreases repeated denial codes in medical billing and improves the accuracy of claim.
Conclusion:
iSolve RCM, the best medical billing company in USA supports healthcare providers to overcome emerging denial codes in medical billing through smart automation, real-time analytics, and professional compliance support. iSolve RCM reduces common denials like CO-16, CO-50, and CO-222 With AI claim scrubbing, denial tracking, and ongoing coder training. It ensures faster reimbursements, fewer rejections, and stronger revenue integrity in 2026.