Precision plays an important role in medical billing. Delays in payments or claim denials can occur from even a small coding error. Modifier 53, a CPT modifier that is important for guaranteeing fair and compliant reimbursement, is one important yet frequently overlooked code.
The modifier 53 description refers to a discontinued process which is one that was started but could not be securely finished due to unexpected patient complications or risks. The 53 modifier indicates that the healthcare provider began a medically essential service but had to stop it to protect the comfort of the patient.
Proper use of modifier 53 improves transparent billing processes in addition to expressing ethical medical judgment. Appropriate reporting through this modifier guarantees that healthcare professionals are paid properly for the portion of work finished while complying to insurance and legal requirements. This blog will try to explore the use of modifier 53 in medical billing.
What Is Modifier 53?
According to Current Procedural Terminology guidelines, Modifier 53 is used to report a discontinued procedure, that is service which was started but ended because of unforeseen circumstances that put the patient’s safety in danger. In other words, the modifier 53 definition explains that while the provider initiated the procedure with the intent to complete it, they made a professional decision to discontinue it to avoid harm or complications.
The 53 modifier helps healthcare providers communicate clearly to payers that the service was medically necessary and partially performed, not abandoned without reason. It guarantees fair payment for the work already done and supports precise reporting of clinical care.
Key points about Modifier 53:
- The procedure must have started but not finished due to complications or risk factors of the patients.
- It reflects a clinical judgment of a provider to discontinue for safety reasons, not convenience.
- Documentation must clearly describe why and when the procedure was stopped.
- It varies from “abandoned” or “incomplete” procedures, which may occur for non-clinical or administrative reasons.
- The modifier 53 description applies only when the healthcare provider has personally started the procedure before discontinuation.
Proper Use of Modifier 53
The 53 modifier is when a procedure has been initiated but ended because of unexpected problems, patient instability, or other situations that make continuation risk. The modifier 53 meaning centers on protecting the security of the patient, permitting that while the service was necessary and begun, completing it would have posed a risk. Healthcare providers often rely on professional medical coding services in the USA to guarantee proper use of Modifier 53 and avoid claim denials.
This modifier 53 description is only applicable when the healthcare provider performs an important component of it, and then ends it in the best interest of the patient. It allows proper reimbursement for the time, effort, and resources that have already been used while maintaining ethical billing standards.
Examples of when to use Modifier 53:
- A colonoscopy is in progress but stopped because of poor patient tolerance or severe discomfort (ICD-10: K63.5 – Polyp of colon).
- A cardiac catheterization is ended after the patient experiences abnormal vital signs.
- A biopsy is ended early because imaging reveals an unexpected complication.
- An endoscopy is stopped midway after detecting a condition that needs immediate stabilization.
Pro Tip: Always document the exact reason and timing for discontinuing a procedure when using Modifier 53. Both the security of patients and reimbursement eligibility are protected by clear and comprehensive notes. Add clinical judgment, the patient’s condition, and any unexpected issues. This guarantees payers know that the service was medically necessary and appropriately discontinued, not abandoned.
When Not to Use Modifier 53
Modifier 53 is important for the reporting procedures that have been stopped, but it should only be used in certain security-related circumstances. improper use of it could end up in claim denials or issues with compliance. The definition of modification 53 makes it very clear that it only applies when a procedure starts and subsequently stops because of unexpected patient challenges, and not for convenience or administrative reasons.
The 53 modifiers should not be used when a service is canceled or interrupted for non-clinical causes such as scheduling delays, equipment issues, or patient choice before anesthesia or incision. These cases do not meet the modifier 53 description because the procedure was never truly started.
Do not use Modifier 53 when:
- A procedure is cancelled before anesthesia, incision, or scope insertion.
- A test or surgery is suspended due to provider or facility scheduling conflicts.
- Diagnostic imaging or lab work is incomplete because of equipment failure.
- The patient refuses the procedure before it begins.
- The case qualifies for Modifier 52 or Modifiers 73/74 instead.
Documentation Requirements for Modifier 53
Accurate use of modifier 53 depends on precise documentation. Precise and comprehensive records are important since these modifiers show that a process was started but not completed for reasons of safety. Clear healthcare records that describe what was done and why it was stopped should always support the modifier 53 description. In addition to guaranteeing ethical billing, this reduces the risk of audits or claim rejection.
When using the 53 modifiers, every detail matters. The provider must record the sequence of events and the specific clinical reason for stopping the procedure. Insurers rely on this documentation to confirm that the service qualifies under the modifier 53 definition and to determine appropriate payment.
Key elements to include in medical records:
- Reason for discontinuation:
Clearly describe the condition of a patient or event that led to stopping the procedure.
- Portion of service completed
Show the stage or percentage of the procedure performed before discontinuation.
- Supporting clinical notes
Include vital signs, intraoperative details, and any interventions made for patient safety.
- Signature and date of the provider
- Authenticate the documentation with the performing provider’s signed note.
Complete and precise documentation supports fair reimbursement and conformance to CPT billing rules by showing professional integrity and the proper use of modifier 53.
Example Scenarios of Modifier 53 Usage
Understanding situations based on real life support clarifies when to apply modifier 53 properly. The modifier 53 description emphasizes that the process must be started and then discontinued because continuing would threaten the safety of the patient. These examples demonstrate proper and improper use to guide in precise billing and documentation.
Proper use of Modifier 53
- The procedure stopped because the patient was upset – The healthcare provider starts the procedure, but it is immediately halted for safety when the patient experiences terrible pain and fluctuating vital signs.
- Surgery stopped due to unexpected bleeding – A doctor starts an abdominal operation, but the team is unable to calm the patient due to severe bleeding.
- Cardiac catheterization stopped midway – The cardiologist stops the procedure halfway through placement when the patient exhibits abnormal rhythm alterations with the goal to prevent more difficulties.
- Discontinued Endoscopy for Airways Risk: When a possibly dangerous airway reaction becomes apparent, the medical professional immediately stops the surgery after unconsciousness.
- Biopsy interrupted owing to allergic response: When a patient suffers an important allergic reaction to a local anesthetic, the physician stops performing the biopsy due to an allergic reaction.
Incorrect use of Modifier 53:
A procedure cancelled before anesthesia or incision because the patient did not arrive on time or the equipment malfunctioned. In this case, the 53-modifier does not apply since the process never began.
These are illustrations to support the modifier 53 definition as it is used only for procedures that were clinically essential, initiated, and discontinued due to surprising complications, not for administrative or scheduling reasons.
Pro Tip: Before applying Modifier 53, double-check that the medical procedure was properly started and stopped only because of patient safety issues. Never employ it for patient preferences, equipment issues, scheduling conflicts, or cancellations. Your claim will be safeguarded from denials and compliance with CPT regulations will be guaranteed by clear documentation that differentiates clinical necessity from administrative or convenience reasons.
Common Denial Codes in 2026 | Errors and Tips for Accurate Billing
Modifier 53 is sometimes misused by even professional medical coders, which may end up in denied claims or issues with compliance. Applying the 53 modifiers to procedures that were cancelled before they started, including those terminated before anesthesia or incision, is one of the most common errors. The modifier 53 demands that the process be started but stopped for patient safety, has been violated by this action. Confusion between modifiers 53 and 52 or 73/74 used in outpatient settings is another common error. Wrong reporting, late payments, as well as audit problems might result from misunderstanding these codes.
To prevent these problems and guarantee effective denial management services, medical billing professionals and coders have to fully understand the modifier 53 description and confirm every claim is supported by proper documentation. The 53 modifier is appropriate in reporting a procedure that started but could not be safely completed. In addition to providing fair compensation and maintaining compliance with CPT and payer rules, proper coding protects provider integrity.
Tips to confirm accurate billing and compliance
- Verify that the procedure was started and discontinued for clinical reasons.
- Do not use modifier 53 for canceled, rescheduled, or incomplete tests due to equipment or patient preference.
- Review operative and progress notes to confirm the event qualifies for discontinuation reporting.
- Maintain clear documentation including the reason, stage of procedure, and signature of the provider.
- Educate staff regularly on modifier 53 usage to stop repetitive billing errors.
- Audit claims periodically to confirm modifier 53 is applied only when supported by medical necessity and proper evidence.
Common Errors and Tips for Accurate Billing
Modifier 53 is sometimes misused by even professional medical coders, which may end up in denied claims or issues with compliance. Applying the 53 modifiers to procedures that were cancelled before they started, including those terminated before anesthesia or incision, is one of the most common errors. The modifier 53 demands that the process be started but stopped for patient safety, has been violated by this action. Confusion between modifiers 53 and 52 or 73/74 used in outpatient settings is another common error. Wrong reporting, late payments, as well as audit problems might result from misunderstanding these codes.
To prevent these problems, medical billing professionals and coders have to fully understand the modifier 53 description and confirm every claim is supported by proper documentation. The 53 modifier is appropriate in reporting a procedure that started but could not be safely completed. In addition to providing fair compensation and maintaining compliance with CPT and payer rules, proper coding protects provider integrity.
Tips to confirm accurate billing and compliance
- Verify that the procedure was started and discontinued for clinical reasons.
- Do not use modifier 53 for canceled, rescheduled, or incomplete tests due to equipment or patient preference.
- Review operative and progress notes to confirm the event qualifies for discontinuation reporting.
- Maintain clear documentation including the reason, stage of procedure, and signature of the provider.
- Educate staff regularly on modifier 53 usage to stop repetitive billing errors.
- Audit claims periodically to confirm modifier 53 is applied only when supported by medical necessity and proper evidence.
Difference Between Important Modifiers
Learning the differences among these CPT modifiers improves timely reporting and billing accuracy. While the modification 53 indicates procedures that have been stopped for reasons of security, extra modifiers describe other circumstances in which a service has been reduced, modified, or discontinued. This is how each is different:
Modifier 52 | Reduced and Fewer Services
When a procedure or service has been shortened but not entirely ceased, Modifier 52 is applied. Because of clinical judgment or patient needs, the provider completes the service, but to a lesser extent than average. Unlike modifier 53, this does not involve a stoppage related to safety.
Key points:
- The procedure is completed, just at a reduced scope or intensity.
- No risk or emergency leads to discontinuation.
- Documentation should explain why the service was limited.
- Commonly used for diagnostic tests or surgical procedures performed in part.
Modifier 53 | Discontinued Procedure
The modifier 53 description applies when a healthcare provider initiates a procedure but discontinues it to stop patient harm. It signals that the service was medically required, initiated, and halted for safety or unexpected complications.
Key points:
- Procedure begins but interrupted because of unexpected potential risks.
- Displays clinical judgment that prioritizes patient safety first.
- Reflects clinical judgment prioritizing patient safety.
- Requires detailed documentation of the event and the portion completed.
- Guarantees partial reimbursement for work performed.
Modifier 52 vs Modifier 53
How does Modifier 52 differ from Modifier 53?
| Modifier 53 | Modifier 54 |
| It is used when a procedure is started, but must be stopped before completion. | It is used when the procedure is fully completed, but the surgeon provides only the surgical care. |
| The procedure is incomplete. | Surgery is complete. |
| Applies mainly to surgical and diagnostic procedures. | Applies to surgeries with global periods. |
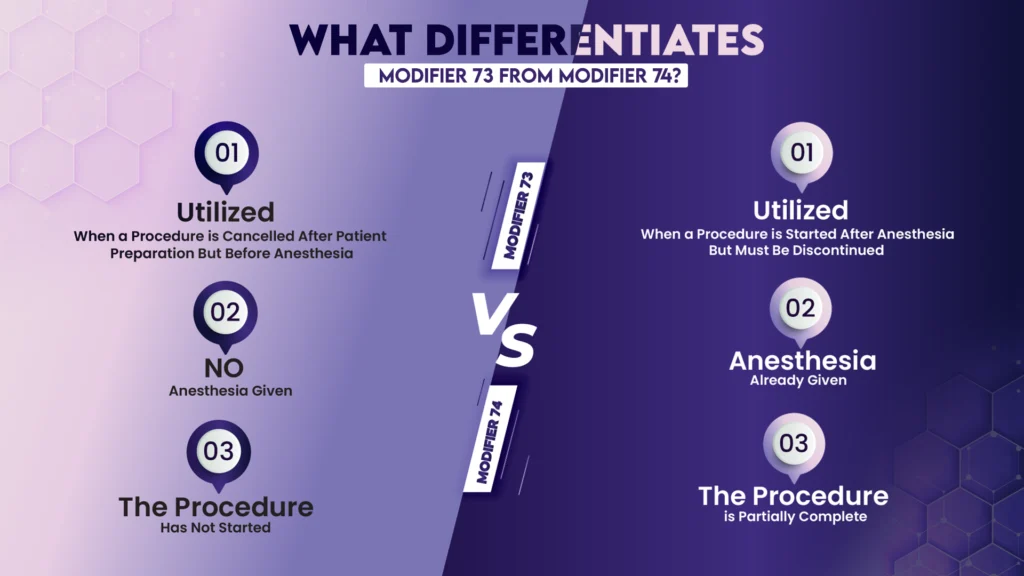
Modifier 73 | Discontinued Outpatient Procedure (Before Anesthesia)
When a procedure stops before the administration of anesthesia, Modifier 73 is utilized in outpatient or ambulatory surgery settings. It fluctuates from modifier 53, as the latter applies once the procedure has actually begun.
Key points:
- Procedure cancelled before anesthesia or surgical start.
- Used only for facility billing, not professional claims.
- Must document the reason for stopping the service.
- No patient safety risk occurred during performance since it did not begin.
Modifier 74 | Discontinued Outpatient Procedure
When an outpatient or ambulatory procedure stops after anesthesia has been delivered or after the procedure started, Modifier 74 is applied. It is similar in concept to modifier 53, but specifically for facility billing rather than the professional service of the healthcare provider.
Key points:
- The procedure began and stopped after anesthesia or scope insertion.
- Used only by facilities, not individual providers.
- Requires documentation of the reason for discontinuation.
- Often applied in same-day surgery or endoscopy centers.
Modifier 73 vs Modifier 74
Important Notes
When a medically necessary procedure must be initiated but terminated for patient safety or unexpected problems, the modifier 53 is an important CPT code that supports fair and accurate reporting. When the modifier 53 description is applied correctly, it communicates that the provider utilized good clinical judgment while continuing to complete an important portion of the treatment. Proper knowledge of modifier 53 supports protecting the health of patients and provider reimbursement.
Verified modifier 53 claims are supported by clear documentation, detailed clinical notes, and a valid reason for discontinuation to sustain compliance and reduce denials. Modifier 53 not only supports ethical billing but also reflects the highest standards of care that put patients first when used correctly.
Pro Tip: Teach all of your staff to tell the difference between Modifiers 52, 53, 73, and 74 with the goal to avoid repeated coding errors. Constant audits and complete documentation of the procedure stage, the reason for discontinuance, and the signature of a healthcare professional are important for proper billing and suitable reimbursement.
How iSolve RCM Supports Accurate Modifier 53 Billing
At iSolve RCM, we are skilled at helping healthcare professionals in precisely, confidently, and compliantly addressing the difficulties of medical billing. Our team of experienced medical coders and billing specialists guarantees that modifiers like modifier 53 are used properly to precisely indicate discontinued procedures and avoid unnecessary claim denials.
We precisely review documentation and verify CPT coding to confirm you receive the reimbursement you deserve. By partnering with iSolve RCM, healthcare providers can not only eliminate billing confusion but also reduce errors. Our proactive approach focuses on education, precision, and transparency, empowering your healthcare practice to focus on patient care while we handle the details of revenue cycle management. Whether it is understanding the modifier 53 definition, correcting underpayments, or preventing compliance risks, iSolve RCM stands beside your healthcare practice as a trusted partner in achieving financial and operational excellence.