The global period is worldwide and is defined as “a specific period of time prior to, during, and after surgery in which certain services are bundled in one global payment.” The global period is measured in days: it may be ‘0,’ “indicating no postoperative period after surgery,” while in other cases it is measured as either ’10 days’ or ’90 days,’ depending upon the type of surgery involved.
Modifiers 58, 78, and 79 are very important for determining which services are provided within the global period but qualify for additional payment. Modifiers 78 and 79 are used for determining whether the treatment is staged or procedure related, unplanned, unrelated procedures, or not related at all to the original surgery performed on the patient.
There is common confusion for both coder and biller regarding how to apply these modifiers correctly. This blog will try to explore which modifier is used for the global period and how this is applicable to a medical coding company in USA.
What Is the Global Period?
The global period is a fixed period post-procedure during which follow-up care is covered by the original reimbursement and cannot be separately billed. This applies to follow-up care post-surgery and is based on 0, 10, or 90 days, depending on the procedure that took place.
Understanding of the Global Surgical Package
Global surgical package refers to a form of bundled payment that is applied in medical billing. It encompasses every service related to surgical care. This package usually covers evaluation prior to the surgical procedure, the surgical procedure, and then care post-surgery.
Types of Global Periods (0-Day, 10-Day, 90-Day)
The modifier global periods of different procedures are 0 day, 10 days, and 90-day global periods. In a 0-day global period, only a day of procedure is considered. In a 10-day global period, postoperative services for a period of ten days after having a surgery. In a 90-day global period, a 90-day global period is experienced after a major operation.
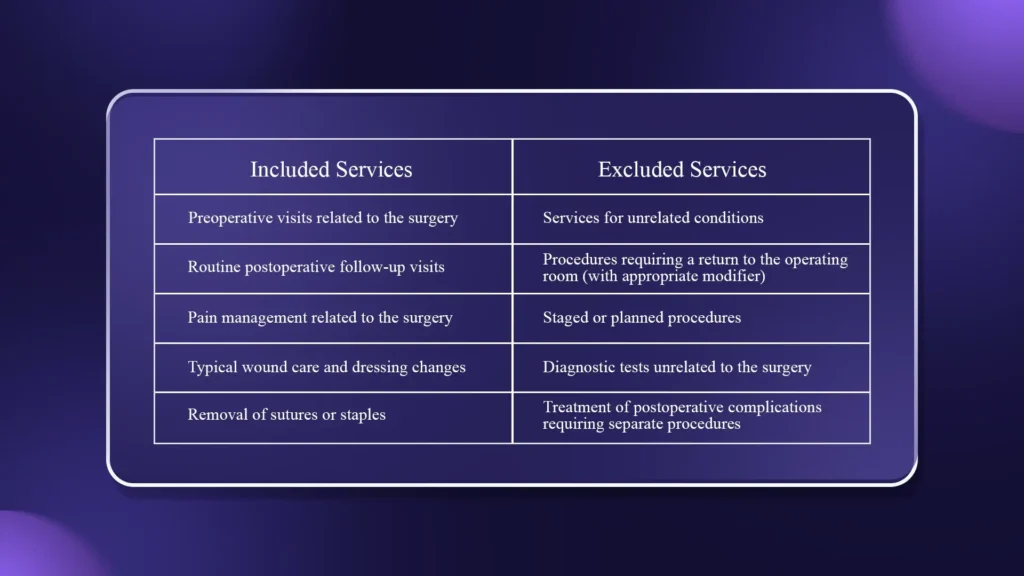
Services Included vs. Excluded in the Global Period
The services rendered during the global period may or may not be separately billable, based on their nature. For outsource medical coding services, understanding this distinction is key to accurate coding and the appropriate use of modifiers.
Why Global Period Modifiers Are Used
Purpose of Using Modifiers During the Global Period
These modifiers are employed during the global period in a manner which indicates whether the service or procedure is either related or unrelated to the original surgery, thus warranting a qualification for payment. These modifiers aid in communicating the situation surrounding the procedure, whether it is a staged, unplanned, as well as an unrelated service which lies beyond the surgery components encapsulated in the global package. This is in a situation where payment for additional services might be rejected through lack of modifiers.
How Modifiers Impact Reimbursement
The appropriate use of modifiers of the global period directly influences reimbursement. For example, a correctly applied modifier may assure full or partial payment for the service, which is not packaged within the global package, while inappropriate use of modifiers may result in denials, reduced payments, or even audits. Modifiers are utilized to differentiate services that represent exceptions to the bundled payment and enable providers to receive adequate reimbursement.
Importance of Correct Modifier Selection
The selection of which modifier to apply is critical in determining compliance as well as correct billing. In some cases, a modifier 58, 78, or 79 explanation of benefit is specific in its application, and any misuse of the modifiers may result in an error in the code as well as loss of funds through disputes over payments.
Pro Tip: It is important to always choose the accurate global period indicator (58, 78, 79) to allow the insurance company to pay the amount in question. This helps in the accurate communication of whether the service, staged, or not related to the original surgery.
Overview of Modifiers 58 vs 78 vs 79
Modifiers 58, 78, and 79 are used to describe specific circumstances under which a procedure is performed during the global surgical period but may be payable separately. Modifier 58 describes a staged or related procedure that is planned or more extensive than the original procedure. Modifier 78 is applied when a patient must return to the operating room unexpectedly to treat a condition related to the original procedure during the postoperative period. Modifier 79 is utilized for procedures that are unrelated to the original surgery and are performed during the global period.
These have different uses. For planned or staged care, the modifier is Modifier 58. Others are Modifier 78 for unexpected complications necessitating extra surgeries. Lastly, Modifier 79 is for unrelated procedures. These three are all important during the global period. Although these are all useful during the global period within which the whole treatment cost is billed, the purpose can differ. Here, the aim of using one can be to extend the former treatment plan.
What is Modifier 58: Staged or Related Procedure
“Modifier 58″-translated in its full form, “Staged or Related Procedure or Service by Current Procedure Terminology (Code) or Medicare Code” – “Performed During the Postoperative Period, Planned or More Extensive Than the Original Procedure.” This particular medical billing code essentially implies that the surgeon assumes there will be another procedure required in the future or when it’s much bigger than the actual procedure conducted initially. For instance, in revision of joint replacements performed.
Modifier 58 is applied in procedures that are planned or staged procedures and are more complex compared to the first surgery. This is usually the case where the second stage of a reconstructive surgery takes place. This will qualify the practitioner for a refund based on the rules and regulations of the respective insurance carrier. It is essential that there is evidence that the service is planned.
What is Modifier 78: Unplanned Return to the Operating Room
Modifier 78 has an official definition of a procedure that occurred in the postoperative period as a complication that requires an unplanned return to the operating room for a related procedure. The use of Modifier 78 reveals that the secondary surgery is medically indicated to correct the complication of the primary surgery.
Modifier 78 is utilized when a patient has a complication from an originally performed surgery that requires another surgical procedure during the global period, such as postoperative bleeding, infection at the surgical site, or other problems that need additional surgery. Reimbursement for procedures billed with modifier 78 is usually reduced because only additional costs for performing the additional surgery are reimbursed, not a full new global period.
Some common billing errors include inappropriate usage of modifier 78 for unrelated procedures, not clearly documenting the complicating issue of record, or substituting this modifier for planned staged procedures, which requires modifier 58.
What is Modifier 79: Modifier for Unrelated Procedure in Global Period
The 79 modifier in medical billing or “Modifier 79” is formally defined as a procedure that occurs during the postoperative period and is not related at all to the initial procedure or this is a modifier for an unrelated procedure in the global period. The modifier essentially informs the insurance company that a separate problem is being addressed and that this new service does not form a part of the initial surgical package for which a billing was made.
This is applicable when the patient requires another procedure due to an issue unrelated to the initial surgery. This could be something like fixing a broken hand when the patient just had knee surgery. When a procedure is billed and modifier 79 is attached to it, it results in billing the procedure fully. The global period resets for this unrelated procedure. The procedure has to be properly documented to ascertain it is unrelated. This is done through the use of diagnosis and operative reports.
According to Minnesota Administrative Rules, CPT modifier 79 is utilized when there is another procedure completed during the postoperative period, and there is documented evidence that it is not related to the initial surgery. Coding for complications that are not listed within the CPT codebook would require the unlisted surgical procedures code with modifier 78, signaling return to the or for related procedures within the modifier global period. Although you can learn about wound care CPT code, billing and coding guidelines for better understanding.
Main Differences Between Modifiers 58, 78, and 79
It is important to grasp the difference between these three suffixes, 58, 78, and 79, in order to bill appropriately within the context of the global period. All three suffixes are used to indicate procedures that happened within the post-op period, with each one having its distinct purpose relative to the index procedure for billing as well as comprehending the meaning behind each suffix. Suffix 58 is used for staged procedures, 78 for return to the OR for complications, while 79 is used for unrelated procedures.
To easily isolate the proper modifier, one needs to consider these significant questions: Was this procedure staged or planned? Was it unplanned but associated with the initial procedure? Or was this procedure unrelated to the initial procedure? Answering these questions places you on track to use the proper modifiers. Here are the following differences of modifier 58 vs 78, modifier 79 vs 78 and 78 vs 79 modifier.
Comparison Table: Modifiers 58, 78, and 79
| Modifier | Purpose | Relation to Original Surgery | Payment/Reimbursement | Global Period Effect |
| 58 | Staged, more complex, or planned procedure | Related or planned continuation of original surgery | Usually full or partial reimbursement | Extends the original global period |
| 78 | Unplanned return to or due to complication | Related or unplanned complication | Reduced payment for additional procedure | Does not reset the global period |
| 79 | Unrelated procedure performed during global period | Unrelated to original surgery | Full reimbursement | Starts a new global period |
79 modifier description, 78 modifier description, modifier 58 description, modifier 79 description with example are used as modifier 58 is applied if there is a planned staged or more complex procedure done by the same practitioner within the global period of the original surgery. This is also used for therapy for a diagnostic surgical procedure. This initiates a new global period, and this is normally 100% payment. This is done with the same diagnosis code or with a different one, but with return to theory as required by Medicare.
Modifier 78 denotes an unplanned return to the operating room for treatment of a complication specifically related to the original surgery, such as infection, hemorrhage, or wound dehiscence. It does not initiate a new global period, and payment is usually restricted to the intraoperative portion, amounting to approximately 70 to 90%. Modifier 79 is applied when there is a completely unrelated procedure done during the global period. It initiates a new global period and is usually paid at about 100%, often for a different diagnosis or anatomical site.
Pro Tip: Ask yourself if the procedure was planned, related, or unrelated to the original surgery. Use 58 for planned/staged, 78 for unplanned complications, and 79 for unrelated procedures in order for proper billing and reimbursement.
Modifier Selection Scenarios
Choosing the appropriate modifier in the global period can be very complex, but examples in scenarios can help in understanding. For example, when the patient comes for the return visit in the case of the second stage of the operation, modifier number 58 is used. If the patient requires the unplanned operation, maybe as a result of the original surgery, then the appropriate modifier is number 78. In the case of the treatment of another, altogether different problem, modifier 79 is used. Furthermore, you can also explore when and how to use modifier 53 in medical billing to understand medifier selection.
The right decision can only be made after answering the following questions posed by the coders: Is this procedure staged or planned?
Did this procedure have any relation with the previous surgery, or was it a complication with regard to that surgery, or was it totally unrelated? The question answers determine if the right modifiers have been assigned.
Common Coding and Billing Errors
The misapplication of global period modifiers is one of the most common reasons for denied claims and delayed payments. These might include using modifier 78 in place of modifier 79, inappropriately using modifier 58, or simply not providing suitable support information to authenticate the procedure.
Other common errors include:
- Charging an unrelated service with a modifier of 78 rather than 79.
- Reporting modifier 58 for unplanned complications instead of staged procedures.
- Voiding critical documents relating the procedure to the original surgery.
- Failure to disclose the medical necessity of staged or related procedures.
- Making assumptions that all postoperative procedures fall within the global period.
- Failure to global period reset when billing unrelated procedures using modifier 79.
- Confusing partial reimbursement rules for modifier 78 versus full payment for modifier 79.
Tips for Accurate Global Period Billing
Billing accurately for the global period involves good documentation, communication, and knowledge of insurance regulations. Using the proper documentation for the procedure, its connection with the primary surgery, as well as its necessity will help in the correct application of the 58, 78, and 79 modifiers.
Best practices include:
- State whether this process is staged, unplanned, or unrelated.
- Describe the operative procedures in detail, including diagnostic codes.
- Keep an active timeline of the original surgery and its post-op period.
- Communicate with the provider to establish the reason and relation to the procedure.
- Payor-specific regulations w/r/t modifier utilization and billing principles.
- Record that all complications and staged surgeries have been done.
- Review coding guidelines often to avoid mistakes and denied claims.
Pro Tip: It is essential to have good documentation of services, specifying whether it is a staged procedure, an unplanned service, or non-related, and keep track of timelines and payor guidelines.
How iSolve RCM support you with Modifier
Knowledge of the major distinctions between modifiers 58, 78, and 79 will play a crucial role in performing effective global period billing. Incorrect usage of the modifiers will not only affect the billing process but will also keep the healthcare organization out of compliance with coding regulations. Using the modifiers correctly, along with the right documentation, communication between healthcare organizations, providers, and the payers, will make it easier for healthcare organizations to manage revenue cycle processes effectively. iSolve RCM helps healthcare organizations manage the process of using modifiers with expert coding advice, claim audits, and live assistance for applying modifiers.
Frequently Asked Questions (FAQs)
Which modifier is used for an unrelated procedure in the global period?
The use of the 79 modifier denotes that the procedure has no connection whatsoever to the original procedure done prior to the global period. The 79 modifier indicates to the insurance company that the current procedure is not included in the global package of the original surgery and is thus eligible for full payment, opening a global period for the newly done procedure.
Does modifier 78 restart the global period?
No, modifier 78 does not restart the global period. It is appended to claim an unplanned return to the operating room related to the original surgery. Payment is usually reduced, and the original global period does not reset.
Does modifier 58 pay at 100%?
Modifier 58 may result in full or partial payment, depending on the payer’s rules and the procedure’s relation to the original surgery. It is used for staged, more complex, or planned procedures, and documentation must clearly justify why the procedure is separate from routine postoperative care.