Appropriate laboratory billing is important for patients, providers, and laboratories to guarantee an uninterrupted dependable care experience. Each investigation is processed safely and patients receive simple statements when billing is performed with precision and clarity. Effective laboratory billing guidelines also promote appropriate reimbursement for the services that patients depend on a daily basis, avoid delays, and stop confusion, an outcome commonly supported by professional medical billing services in USA. By keeping each procedure carefully recorded and properly classified, labs can focus more on producing reliable findings and less on correcting unnecessary mistakes.
Financial stability and compliance are also seriously affected by clear lab billing guidelines. Comprehensive documentation helps coverage decisions and medical necessity, while precise coding assists insurance plans in properly assessing claims. By lowering the potential of denials while offering patients with peace of mind, these actions assist the system as a whole. By complying to CMS laboratory billing requirements, laboratories have the assurance to fulfill requirements set by the government, safeguarding patients and supporting providers in getting regular reimbursement for their time and effort.
Each type of laboratory facility can adhere to the requirements that apply to its workflow by understanding the structure of clinical laboratory billing guidelines, reference laboratory billing guidelines, independent laboratory billing guidelines, and physician billing guidelines for laboratory services. The care team’s communication gets better and unnecessary delays and rework goes away when a suitable billing approach is implemented in a suitable environment. This blog will cover rules, guidelines, modifications and errors of laboratory billing.
Essential Terms Every Lab Professional Should Know
Learning certain terminologies will allow you to navigate laboratory billing and guarantee precise and prompt processing of claims. These important terms assist labs to guarantee proper reimbursement and compliance, from independent facilities to clinical and reference labs.
- Each lab procedure and tests of a patient are recognized by standardized codes such as CPT also known as Current Procedural Terminology.
- Equipment, lab supplies, along with specific procedures that are not regulated by CPT are usually referred to using coding systems such as Healthcare Common Procedure Coding System (HCPCS).
- Federal laws that confirm laboratories follow quality and safety guidelines or procedures is termed as Clinical Laboratory Improvement Amendments (CLIA).
- A unique identification number such as National Provider Identifier that healthcare providers receive so that billing and claim forms can be detected.
- A set of diagnostic codes which support insurance claims and explain the medical importance of each test is called The International Classification of Diseases, or ICD-10.
Comprehending and implementing these terms properly promises simple, compliant, and consistent laboratory billing. In addition to promoting proper reimbursement, complying to established lab billing requirements through proper coding and documentation also prevents errors, decreases delays, and improves the patient experience. The foundation for effective laboratory billing methods in a variety of laboratories is mastery of this main terminology.
Pro Tip: Make sure that you understand the basic concepts utilized in lab billing, which include CPT, HCPCS, CLIA, NPI, and ICD-10. Addressing them makes it simpler to code and file tests properly, eliminate errors, and accelerate the approval of claims.
Essential Laboratory Billing Rules
A variety of fundamental rules must be followed for proper laboratory billing in order to promise effective compliance and suitable reimbursement. These rules permit laboratories to provide reliable support while maintaining care focused on patients.
Medical Necessity Requirements
There must be a compelling clinical reason for each laboratory test. It is obvious that the test must be performed for diagnosis, treatment, or monitoring when the medical necessity is noted in the patient’s file. Following this approach lowers claim denials or delays and adheres to CMS laboratory billing guidelines.
Correct Coding and Documentation
Each test is precisely represented on a claim when CPT, HCPCS, and ICD-10 codes are utilized for proper coding. Comprehensive documentation describing the goal of the testing and the outcomes supports the codes. Coding errors or poor documentation can end up in claims getting denied, reimbursement being delayed, or issues with compliance.
Appropriate Use of Modifiers
Modifiers convey important information about special circumstances, such as repeated tests or additional procedures. Correct application of modifiers guarantees payers clearly understand the services provided and decreases unnecessary claim denials.
Patient Information and Insurance Verification
Claims get submitted to the proper payer and processed promptly when patient eligibility, coverage, and demographics are checked prior to their submission. Comprehensive information allows timely payment and a better patient experience. Laboratories may properly comply with laboratory billing standards and maintain proper operations and reimbursement by closely tracking coding, medical necessity, modifiers, and insurance records.
CMS Laboratory Billing Guidelines
Appropriate billing and compliance are closely interconnected in the intricate environment that laboratories operate. Labs may deal with this complexity by following CMS laboratory billing requirements, which promise proper test billing, fast claim processing, and understandable statements for patients.
CMS guidelines rely on Medicare coverage rules. Strong medical necessity criteria must be satisfied for each service, and not every test is paid. Each order must be carefully reviewed by labs to guarantee sure it meets coverage regulations. In addition to avoiding claim denials, this diligence guarantees patients that all required tests are correctly documented and billed.
Appropriate and coding are equally important. The diagnosis, test results and clinical explanation of the patient must all be incorporated into each claim. Effective application of CPT, HCPCS, and ICD-10 codes, commonly guaranteed by a medical coding company, enables uninterrupted claims review.
CLIA certification also impacts CMS billing. To verify that they follow federal quality and safety standards, laboratories need to keep up their latest certification. Without it, claims face a chance of being rejected, which could result in a negative effect on payment and operational stability.
CMS constantly updates its fee schedules. Laboratories can file accurate claims, execute necessary process changes, and guard their revenue by staying ahead with evolving billing trends. Laboratories are better equipped to maintain compliance, get the right compensation, and provide patients with a clear and fair billing experience when these regulations are closely adhered to.
Clinical Laboratory Billing Guidelines
1. In-House Clinical Lab Billing Rules
As soon as a test is ordered, billing starts. Labs need to make sure the test is medically necessary, correctly documented, and compliance with payer and federal laws. At that stage, timely reimbursement and effective claims processing rely on clear documentation.
2. Specimen Handling and Processing Codes
Proper handling of samples is a requirement for effective billing. All samples must be appropriately documented and inspected at each step of the procedure for testing. Assigning the sample to the appropriate CPT, HCPCS, or ICD-10 codes may render it possible for patients to get a thorough representation of the complete process, which reduces delays or claim denials.
3. Routine vs. Diagnostic Testing
It is really important to differentiate between routine and diagnostic tests. While diagnostic tests demand further documentation to show medical need, routine testing is reimbursed according to usual protocols. Laboratories may preserve effectiveness and follow lab billing guidelines by correctly identifying and billing these tests.
4. Guaranteeing Compliance and Patient Transparency
Integrating correct coding, appropriate specimen processing, and suitable billing guarantees compliance, secures reimbursement, and offers patients a clear and reliable billing. Clinical laboratories are able to provide exceptional healthcare to patients while operating in a professional manner by performing these steps.
Reference Laboratory Billing Guidelines
Tests which are referred from other labs or healthcare providers are managed carefully via reference laboratories. For these tests, proper billing is necessary to guarantee proper reimbursement and compliance. It is simpler to submit and process claims correctly when referrals, evaluations, and patient data are properly recorded.
Key aspects of reference laboratory billing include:
- Billing for Referred-Out Tests
Understanding when and how to bill for services offered by different laboratories is important. Claims are precise and on time when the referral and evaluation are properly documented.
- Billing Responsibilities – Sending vs. Performing Labs
Normally the testing lab bills for the actual analysis, while the sending lab performs the initial collection of samples and documentation. If roles had been clearly established, duplicate billing, denials, and issues with compliance could be prevented.
- Proper Use of Reference Lab Codes
Implementing CPT, HCPCS, or ICD-10 codes appropriately guarantees that claims precisely represent services, are resolved effectively, and comply with reference laboratory billing rules.
- Maintaining Compliance and Transparency
Reference laboratories can preserve compliance, promote reimbursement, and guarantee sending labs and patients fair consistent billing by complying with these rules. This is accomplished by correct referral documentation, different responsibilities, and suitable coding.
Pro Tip: Always makes sure that assessments get done effectively, completely recorded, correctly and effectively coded. Before submitting claims, reviewing patient and insurance company information facilitates fast reimbursement and assists in preventing denials.
Independent Laboratory Billing Guidelines
Independent laboratories which include freestanding and non-hospital laboratories must adhere to specific rules and regulations in order to guarantee proper billing, compliance, and timely reimbursement. This is how they tackle it:
Step 1: Learn the Lab Requirements
Proper billing, coding, and documentation standards have to be satisfied by independent and freestanding labs. Issues are prevented by making sure every claim correctly represents the test and patient information.
Step 2: Adhere to Regulations
Independent labs must be met by federal regulations like CLIA certification and follow state-specific rules. Compliance to these regulations allows appropriate claim processing and helps in avoiding fees.
Step 3: Navigate Unique Billing Scenarios
Some situations deserve exceptional care:
- Tests that come from healthcare facilities.
- Multiple tests for the exact patient.
- Specialized or exceptional testing services.
Step 4: Guarantee Precision and Transparency
By following these requirements, understanding standards, staying compliant, and coding appropriately, independent laboratories can sustain appropriate billing, increase reimbursement, and deliver patients an honest and transparent professional experience.
Physician Billing Guidelines for Laboratory Services
Physicians must follow precise rules when billing laboratory services to ensure compliance, accurate reimbursement, and clear documentation. Knowing when to bill is the first essential step. Physicians may submit claims for tests they perform or order; however, the diagnosis and medical necessity for each test must be properly documented to ensure claims are accepted without unnecessary delays an important function supported through effective Revenue Cycle Management Services.
In-office and point-of-care testing require careful attention to billing standards. Tests performed within a provider’s office must comply with specific regulations. Assigning the correct CPT, HCPCS, and ICD-10 codes helps avoid duplication with external laboratory claims and ensures procedures are reimbursed appropriately.
Split billing situations can be challenging and demand accurate documentation. Providers must clearly record which components of a procedure were performed by the healthcare professional and which were completed by the laboratory. Proper coding reduces errors, lowers the risk of claim denials, and ensures all parties receive accurate reimbursement.
By following physician billing guidelines for laboratory services, healthcare providers can maintain full compliance, support timely reimbursement, and deliver a clear and efficient billing experience. Appropriate coding, thorough documentation, and careful management of in-office and split billing processes remain essential for accurate laboratory billing.
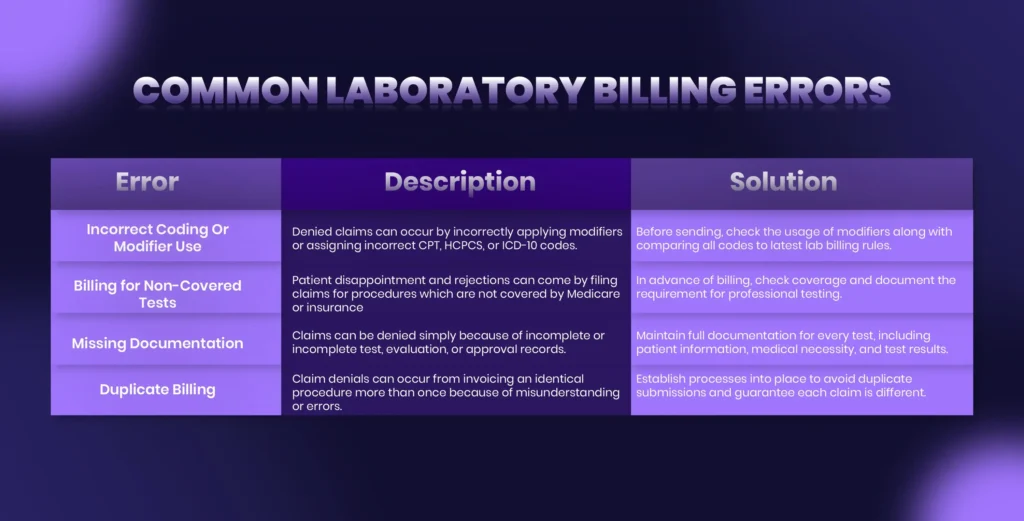
Common Laboratory Billing Errors
Updates in Laboratory Billing
Laboratory billing keeps changing from year to year, and that makes it important for healthcare providers to stay updated with new rules and regulations. The most recent modifications include new CPT and HCPCS codes, fluctuations in CMS billing policies, improvements to the reimbursement rates, and updates to federal and state requirements such as CLIA. Understanding these updates enables laboratories to stay compliant, reduce claim denials, and secure correct reimbursement.
Top Healthcare Practices for Compliance
A few basic steps must be followed for proper laboratory billing:
- Use of billing software
Automation tools help standardize claims, catch mistakes, and maintain dependable records.
- Regular audits
Internal reviews recognize coding or documentation issues early and protect against audits and denials.
- Staff training
Keeping billing staff up to date on paperwork changes and coding prevents errors.
- Proper coding
Appropriate use of CPT, HCPCS, and ICD-10 codes guarantees clean claims and adequate reimbursement.
Pro Tip: Guarantee that all test records are complete, properly code each claim, and confirm insurance coverage before submission. Proper claims and timely reimbursements are guaranteed by regular audits and training for staff.
How iSolve RCM Helps Support Complete Laboratory Billing Guidelines
iSolve RCM improves laboratory billing simpler by assisting labs meet requirements and avoid frequent mistakes. The system tracks the latest and most recent modifications in CPT, HCPCS, ICD-10, CMS, and CLIA, checks codes, and reviews claims before they send them out. These assist labs send clean claims, reduce denials, and get paid on time. iSolve RCM enables labs to concentrate on patient care while maintaining their billing processes precise, compliant, and simple to handle through improved organization, clear documentation, and fewer errors.