Eligibility Verification
& Prior Authorization
Verify Benefits and Eligibility for your Patients in the fastest way possible

Verify Benefits and Eligibility for your Patients in the fastest way possible

Prior authorization refers to the eligibility verification process that allows practices to submit and recoup approved claims to optimize cash flow. Poor prior authorization processes can lead to the exact opposite of what you want – increased denials and decreased revenue. To receive payments for the services rendered, healthcare providers need to verify each patient’s eligibility and benefits before the patient’s visit. Some estimates indicate that as many as 75% of the claims getting denied are on account of the patient not being eligible for the services rendered by the healthcare provider. Unfortunately, it is one of the most neglected processes in the revenue cycle chain.
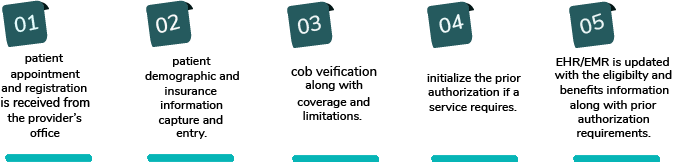
iSolve RCMs Eligibility verification and prior authorization services offer:
We at iSolve RCM offer our providers the most effective automated workflow to bypass patient eligibility denials. Our services ensure a hassle-free experience for both the providers and their patients. We ensure comprehensive eligibility checks through automation tech prior to services rendered.
Through our system, the provider is immediately informed of pending patient responsibilities, Co-Pay, and other dues. We provide an aggressive check system where all patient’s statuses are verified.